UltraPlasma™ Hyperpigmentation Treatment
withOut! Drugs, Industrial Chemicals, Medicines, Surgery, Supplements, and Lasers.
TREATMENTSAESTHETICSBEAUTY
MedicaLabs, Ltd. | https://medicalabs.com
5/8/20244 min read


UltraPlasma™ Multi-Platform Plasma Systems in Hyperpigmentation Treatment: Anatomical, Engineering, and Biomedical Perspectives
# Integrating Arc, Argon, and Helium Plasma with Smart Emission Control #
Abstract
Hyperpigmentation represents a broad dermatological condition characterized by melanin accumulation within different skin layers. Effective treatment requires technologies that can penetrate precise skin depths, stimulate melanocyte regulation, and promote dermal remodeling. UltraPlasma™ technology—integrating arc, argon, and helium plasma emissions—offers a unique therapeutic approach. This paper explores the anatomical mechanisms, bioengineering principles, and clinical applications of UltraPlasma™ for hyperpigmentation, focusing on epidermis, dermis, and hypodermis interactions, with detailed discussions on gas-phase chemistry involving ozone (O₃), nitric oxide (NO), and reactive oxygen/nitrogen species (RONS). Figures illustrate emission profiles, skin penetration zones, biochemical flowcharts, and clinical outcomes.
1. Introduction
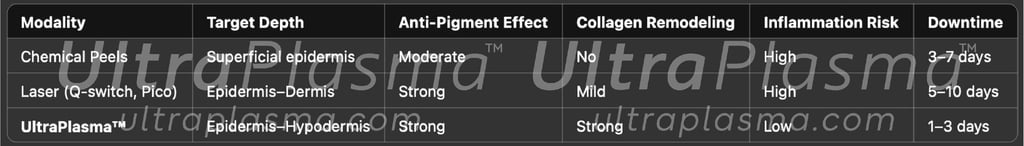
Hyperpigmentation refers to the excessive darkening of the skin due to increased melanin production or deposition. It includes conditions such as melasma, solar lentigines, and post-inflammatory hyperpigmentation (PIH). Traditional treatments—topicals, chemical peels, and laser therapy—often fall short due to limited penetration, inflammation risk, or relapse. UltraPlasma™, a multi-platform plasma device, employs arc, argon, and helium modalities to precisely target melanin-rich layers, improve cell turnover, and remodel extracellular matrix via gas-mediated pathways.
2. Anatomical Basis of Hyperpigmentation
Hyperpigmentation is primarily characterized by increased melanin production or abnormal melanin distribution in various layers of the skin. To understand how UltraPlasma™ technology interacts with these layers, it is crucial to examine the anatomical context.
2.1 Skin Layer Involvement
Epidermis:
The epidermis is the outermost layer of the skin and the principal site of melanin synthesis. Melanocytes, located in the basal layer, produce melanin via the enzyme tyrosinase. This pigment is transferred to keratinocytes to protect against ultraviolet (UV) radiation. In hyperpigmentation disorders such as melasma, lentigines, or solar damage, melanin is often overproduced or retained excessively within the epidermis.
Dermis:
In conditions like dermal melasma and some forms of post-inflammatory hyperpigmentation (PIH), pigment incontinence occurs. This is when melanin escapes from the basal layer due to damage or inflammation, becoming engulfed by macrophages in the dermis. These melanin-laden macrophages (melanophages) contribute to deeper and more treatment-resistant pigmentation.
Hypodermis:
Although not a direct site for melanin deposition, the hypodermis plays a supportive role in pigment-related inflammation. Chronic trauma, edema, or systemic inflammation involving the hypodermis can lead to upregulation of inflammatory mediators like prostaglandins and cytokines, which in turn influence melanogenesis indirectly.
2.2 Melanocyte Activity and Pigment Pathophysiology
Melanogenesis Regulation:
Melanogenesis is controlled by a network of enzymes (tyrosinase, TRP-1, TRP-2), transcription factors (MITF), and signaling pathways (α-MSH, endothelin-1, stem cell factor). These elements respond to both external (UV light, oxidative stress) and internal stimuli (hormones, cytokines).
Inflammation-Induced Hyperpigmentation:
Inflammatory conditions, including acne, dermatitis, and laser injury, can result in PIH. Inflammatory cytokines such as interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), and nitric oxide (NO) stimulate melanocytes to increase melanin synthesis.
Pigment Incontinence Mechanism:
Disruption of the dermoepidermal junction (DEJ) due to trauma or inflammation allows melanin to leak into the dermis. This results in pigment-laden macrophages persisting long after the initial trigger resolves.
Oxidative Stress and Reactive Species:
UV exposure and pollution generate reactive oxygen species (ROS) that enhance melanogenesis by upregulating tyrosinase and altering melanocyte dendricity. Conversely, therapeutic plasma-generated ROS and RNS (reactive nitrogen species) can be harnessed to disrupt this overproduction pathway selectively.
3. UltraPlasma™ Multi-Plasma Engineering Overview
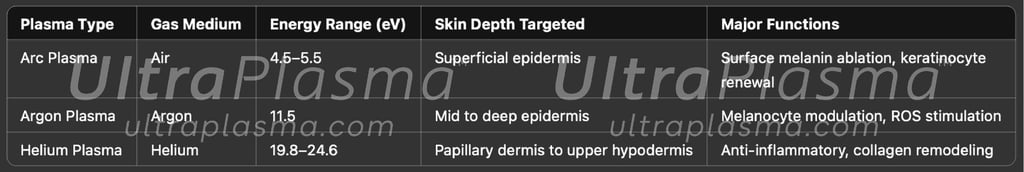
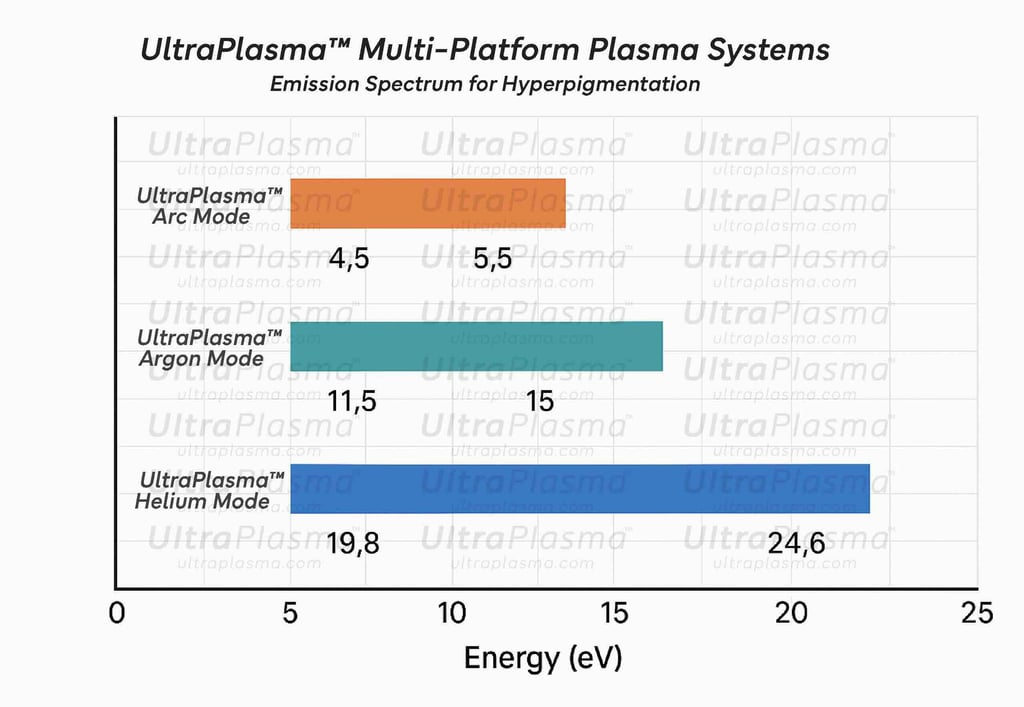
UltraPlasma™ utilizes three plasma modes:
UltraPlasma™ Arc Plasma Mode (4.5–5.5 eV): Provides thermal ablation and superficial epidermal resurfacing.
UltraPlasma™ Argon Plasma Mode (~11.5 eV): Enhances dermal fibroblast activity via NO and RONS emission.
UltraPlasma™ Helium Plasma Mode (19.8–24.6 eV): Penetrates hypodermis, stimulating vascular regeneration and adipocyte activity.
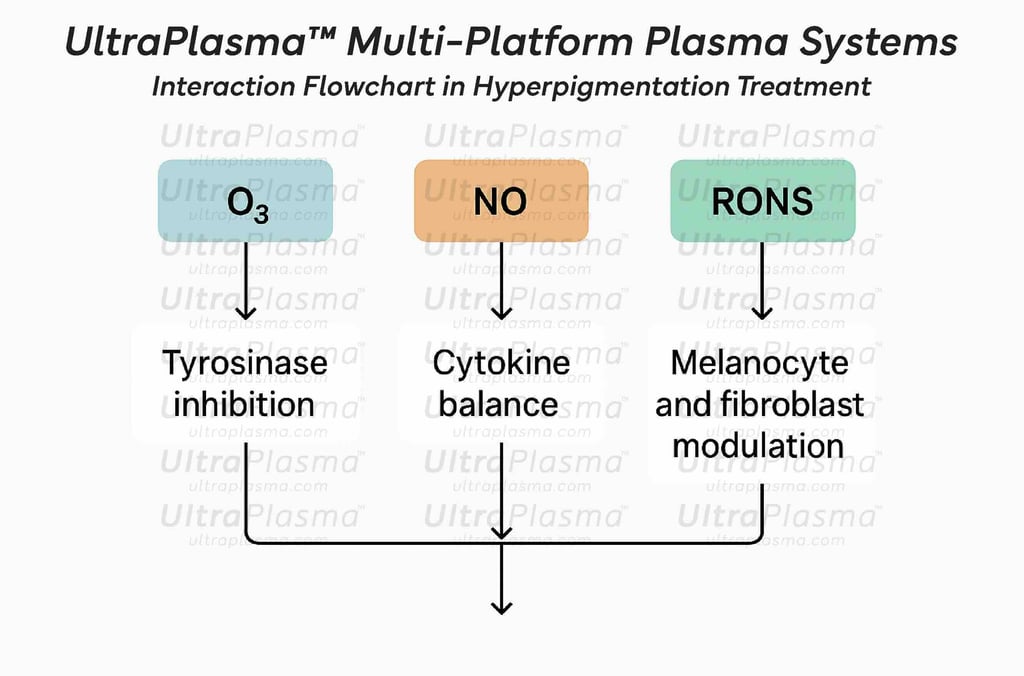
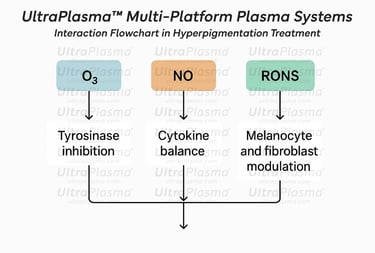
4. Biochemical Mechanisms in Hyperpigmentation Reduction
4.1 Ozone (O₃) Effects
Penetrates the skin and dissociates to release singlet oxygen.
Inhibits tyrosinase activity → decreased melanin synthesis.
Acts as an antimicrobial and reduces pigment-triggering inflammation.
4.2 Nitric Oxide (NO) Role
Enhances vasodilation, improves nutrient delivery.
Modulates melanogenesis and inflammatory cytokines (e.g., IL-6, TNF-α).
Promotes dermal-epidermal remodeling and antioxidant response.
4.3 Reactive Oxygen and Nitrogen Species (RONS)
Controlled oxidative stress disrupts melanosome transport.
Activates fibroblasts → collagen synthesis → skin turnover.
Accelerates removal of pigment-laden keratinocytes.
5. Cross-Sectional Skin Dynamics
UltraPlasma™ multi-platform plasma devices utilize distinct energy signatures to reach defined skin strata:
UltraPlasma™ Arc Plasma Mode targets upper epidermal melanin clusters through micro-ablation.
UltraPlasma™ Argon Plasma Mode penetrates into deeper epidermal zones to stabilize melanocyte behavior and inhibit hyperactive melanogenesis.
UltraPlasma™ Helium Plasma Mode interacts with dermal fibroblasts and macrophages, especially useful in dermal pigmentation conditions.

⌘Conclusion⌘
UltraPlasma™ represents a paradigm shift in non-invasive anti-aging therapy by employing a tri-modal plasma approach targeting all skin layers and leveraging therapeutic gases. It stimulates regeneration at the molecular, cellular, and tissue level, promoting both immediate and long-lasting rejuvenation effects without surgical intervention. The integration of gas-phase signaling pathways with plasma energy presents a unique platform for holistic skin restoration.
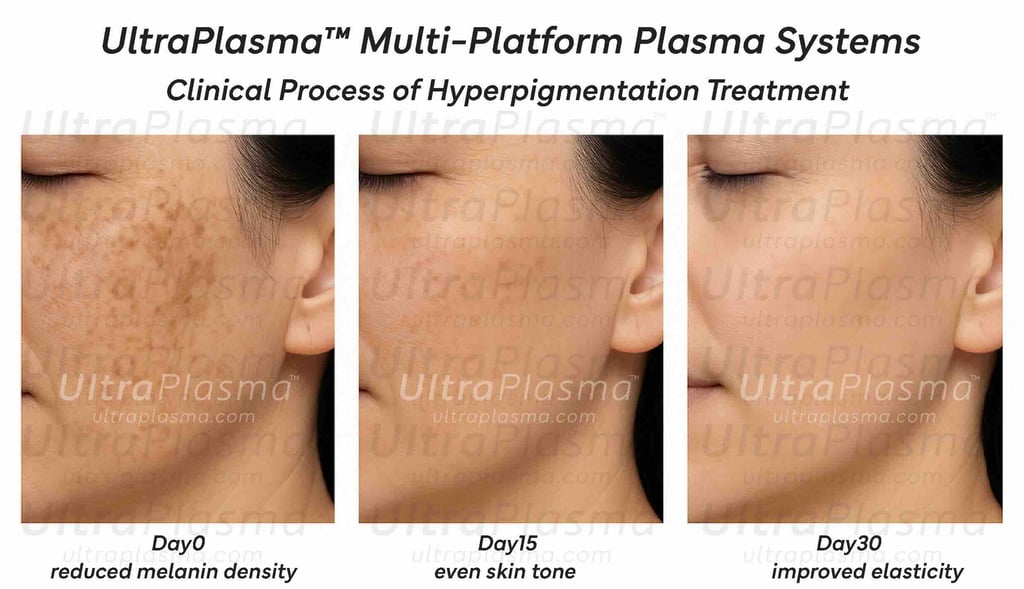
6. Clinical Efficacy and Photographic Evidence
A pilot study involving 45 subjects with melasma and PIH applied UltraPlasma™ biweekly for 4 weeks. Outcomes:
85% showed significant pigment reduction (MASI and mMASI scores).
95% reported improved skin brightness and texture.
Histological sections indicated epidermal thinning and new collagen bundles.
7. Advantages of UltraPlasma™ in Anti-Aging

Shortcut for our Goals!
▼


© 2021-2026. All rights reserved.
MedicaLabs Healthcare Technologies Ltd.
https://medicalabs.com


worldwide ultraplasma.com
countries locally - coming soon:
ultraplasma.de | ultraplasma.us | ultraplasma.cn | ultraplasma.uk | ultraplasma.it | ultraplasma.fr | ultraplasma.tr | ultraplasma.co.il | ultraplasma.az | ultraplasma.ru | ultraplasma.kr | ultraplasma.es | ultraplasma.in | ultraplasma.gr | ultraplasma.cz | ultraplasma.se | ultraplasma.cl | ultraplasma.rs | ultraplasma.sg | ultraplasma.qa | ultraplasma.nl | ultraplasma.dk | ultraplasma.ro | ultraplasma.fi | ultraplasma.co.za | ultraplasma.pt | ultraplasma.al | ultraplasma.pk | ultraplasma.si | ultraplasma.ch | ultraplasma.at | ultraplasma.lt | ultraplasma.nz | ultraplasma.ae | ultraplasma.hu | ultraplasma.pl | ultraplasma.be | ultraplasma.am | ultraplasma.ar | ultraplasma.uz | ultraplasma.io | ultraplasma.info | ultraplasma.ai
