UltraPlasma™ Breast Reconstruction (Plasma Mastopexy)
withOut! Drugs, Industrial Chemicals, Medicines, Surgery, Supplements, and Lasers.
AESTHETICSBEAUTY
MedicaLabs, Ltd. | https://medicalabs.com
5/8/20249 min read


Breast Reconstruction, Shaping, and Plasma Mastopexy via UltraPlasma™ Multi-Platform Arc, Argon, and Helium Plasma Systems: An Integrated Anatomical and Engineering Approach
# Integrating Arc, Argon, and Helium Plasma with Smart Emission Control #
Abstract
The demand for non-invasive and minimally invasive procedures in breast reconstruction, contouring, and lifting has led to the development of novel energy-based technologies. This article presents an in-depth academic, anatomical, and engineering-based analysis of UltraPlasma™, a multi-platform system integrating arc, argon, and helium plasma modalities. Each plasma type offers distinct energy profiles and gas-phase interactions tailored to the epidermis, dermis, and hypodermis. Particular emphasis is placed on plasma mastopexy, a non-surgical breast lifting technique utilizing controlled subdermal contraction and collagen remodeling. The biological effects of ozone (O₃), nitric oxide (NO), and reactive oxygen and nitrogen species (RONS) are explored in relation to skin tightening, angiogenesis, and extracellular matrix regeneration. By employing energy- and gas-specific interactions with soft tissue layers, UltraPlasma™ enables gradual, scar-free improvement in breast contour, volume support, and dermal integrity. This multi-layered plasma approach offers a paradigm shift in aesthetic and reconstructive breast procedures, bridging engineering precision with regenerative medicine.
1. Introduction
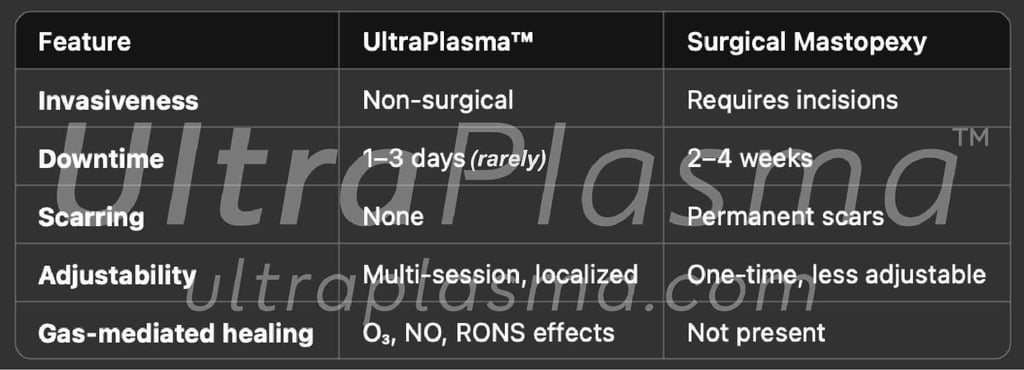
Breast aesthetic and reconstructive procedures—especially those focused on volume restoration, contouring, and lifting—have traditionally relied on surgical interventions. However, non-invasive or minimally invasive approaches are gaining traction due to reduced morbidity, faster recovery, and improved tissue quality. UltraPlasma™, a multi-platform plasma technology integrating arc, argon, and helium plasma systems, enables layered, gas-mediated bioactivation of skin and subcutaneous tissues.
This article explores the anatomical basis, engineering principles, and clinical applications of UltraPlasma™ in breast reconstruction, shaping, and particularly plasma mastopexy (non-surgical breast lift), with a focus on epidermal, dermal, and hypodermal responses, alongside interactions with ozone, nitric oxide (NO), and reactive gas species.
2.Anatomical Framework for Breast Contouring
Understanding the layered structure of the breast and its suspensory and connective framework is essential for the safe and effective application of energy-based technologies such as UltraPlasma™. The breast is not only a glandular and adipose organ but also a mechanically dynamic structure supported by ligaments, fascia, and dermal anchoring systems that respond to external stimuli such as thermal or electromagnetic energy.
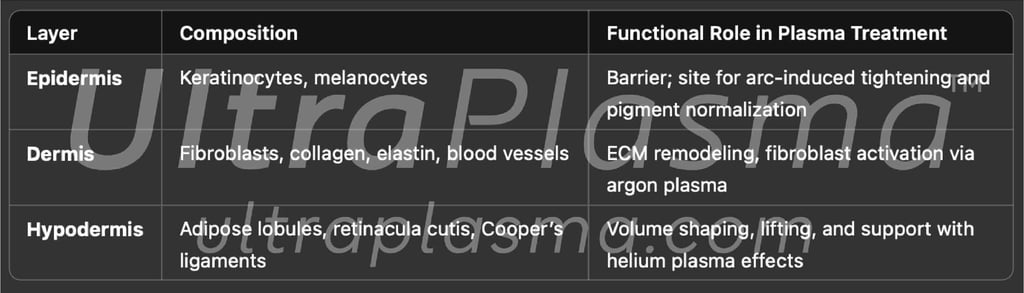
2.1. Layered Architecture of the Breast Skin and Subcutaneous System
3. UltraPlasma™ Technology Overview
3.1. Platform Description
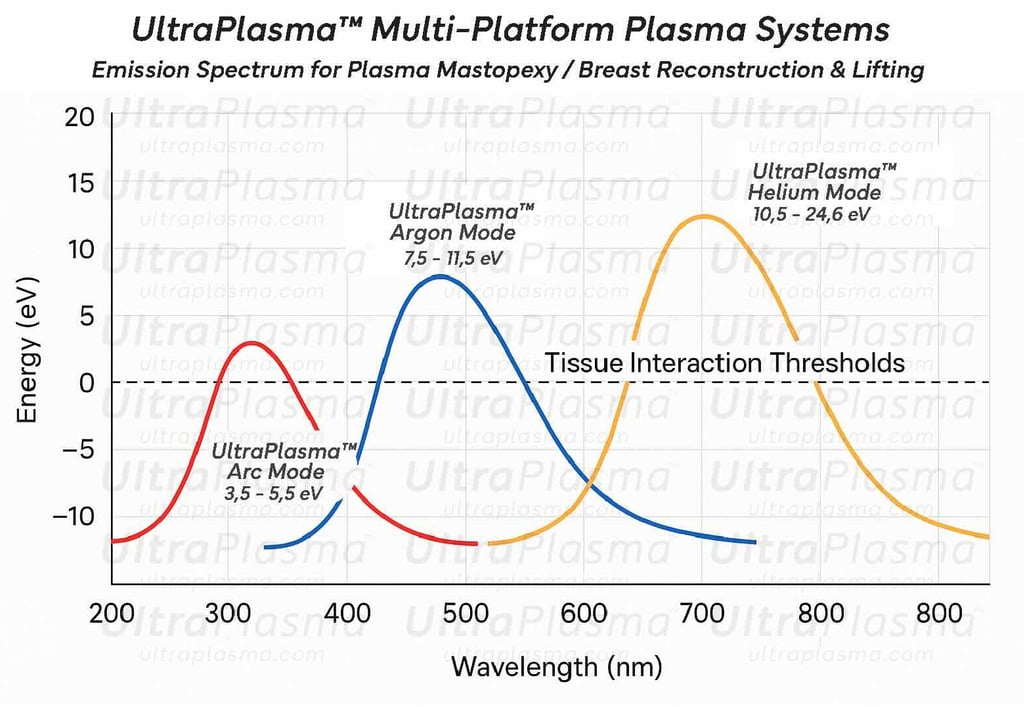
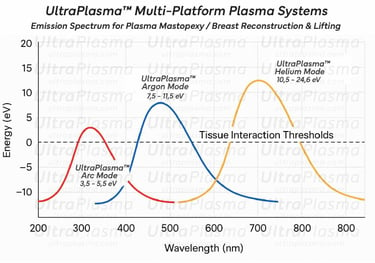
UltraPlasma™ combines:
Arc Plasma (3.5–5.5 eV): Delivers micro-sparks targeting the epidermis, inducing immediate skin contraction and sterilization.
Argon Plasma (7,5 - 11.5 eV): Stimulates dermal ECM remodeling with minimal heat diffusion.
Helium Plasma (10,5–24.6 eV): Penetrates into the hypodermis, initiating subdermal contraction and tissue lifting via selective thermal diffusion.
3.2. Control Systems
Variable frequency modulation (VFM): Adjusts pulse width and frequency per layer.
Sensor-driven impedance mapping: Prevents overtreatment or burns.
Gas-specific nozzles: Optimize flow rates (0.2–1.0 L/min for argon/helium) and maintain plasma focus.
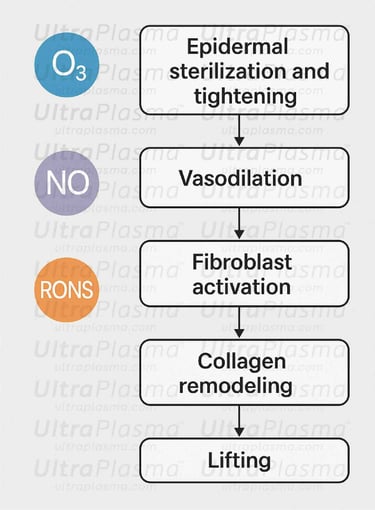
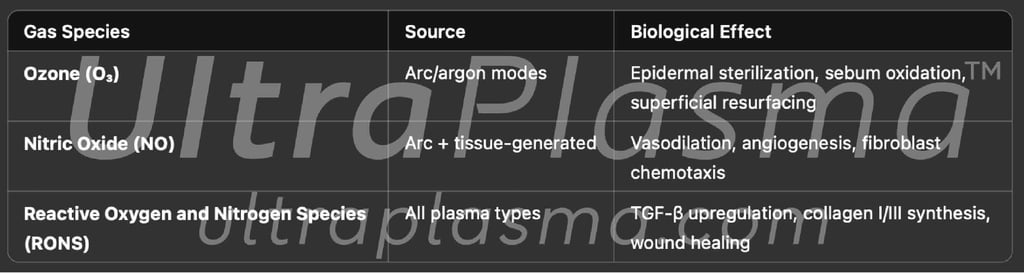
4. Plasma-Gas Bio-Interactions
Plasma treatment not only delivers controlled thermal or electromagnetic energy but also acts as a source of biologically active gases that interact with cells, extracellular matrix (ECM), and vasculature. UltraPlasma™ technology is particularly effective due to its engineered capability to regulate these plasma-generated gases for therapeutic effects at multiple skin depths. This section outlines the key gas species involved and their specific bioactivity in skin tightening, tissue regeneration, and lifting applications.
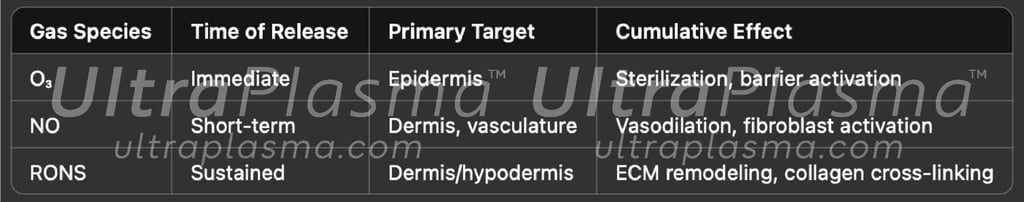
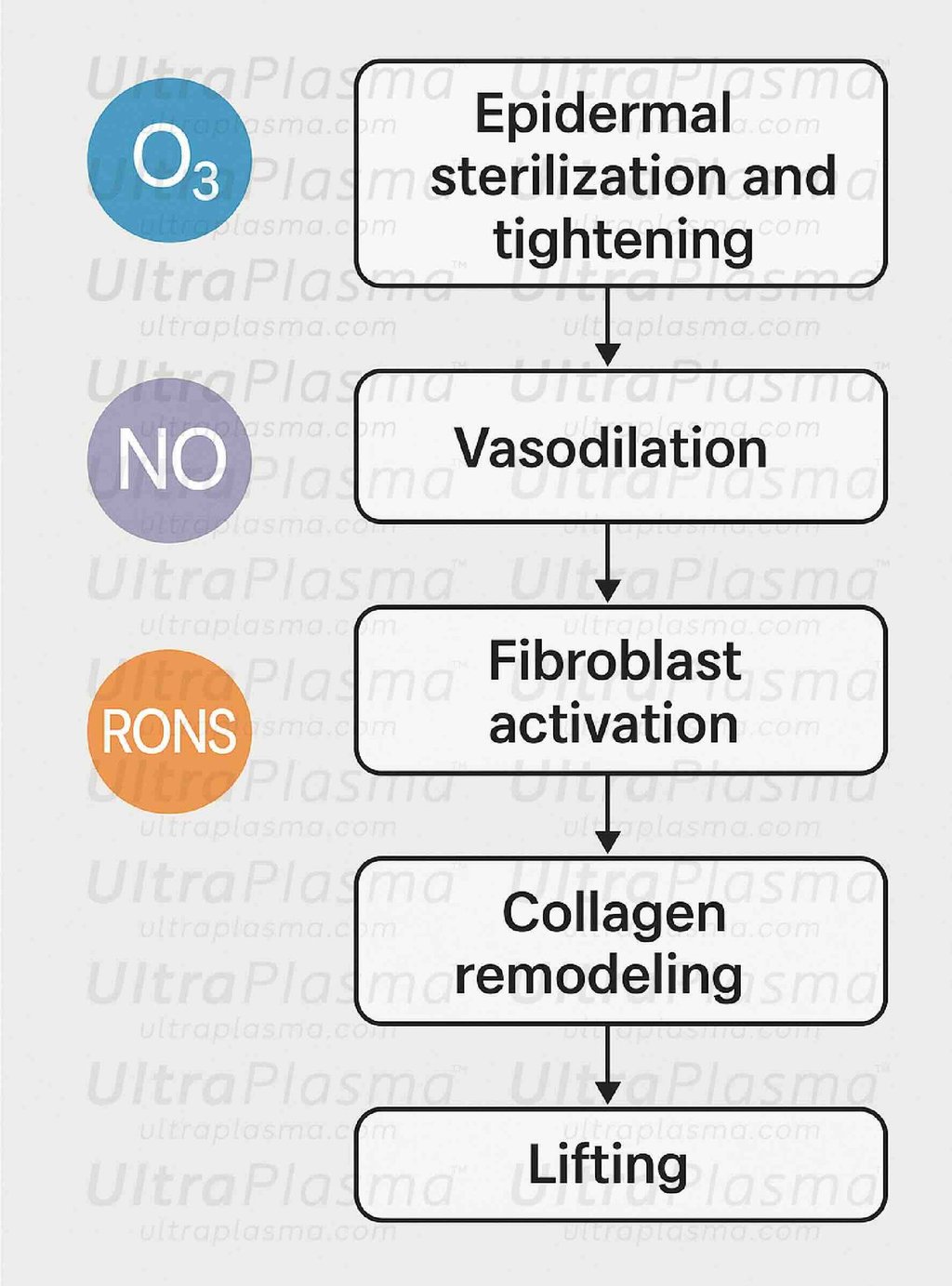
4.1. Ozone (O₃)
Origin: Primarily generated in arc plasma mode via the ionization of atmospheric oxygen (O₂ → O₃).
Tissue Target: Epidermis and upper papillary dermis
Biological Effects:
Antimicrobial Action: Strong oxidative properties lead to the rapid destruction of bacterial membranes, fungal spores, and viruses. This supports a sterile healing environment, especially relevant in post-operative or mastopexy care.
Lipid and Sebum Oxidation: Reduces sebaceous gland overactivity, particularly in the inframammary and areolar zones.
Stratum Corneum Renewal: Mildly exfoliates the outermost skin layer, promoting keratinocyte turnover and enhancing skin texture and tone.
Preconditioning Effect: Transient oxidative stress induces adaptive antioxidant responses in epidermal cells, upregulating protective enzymes such as superoxide dismutase (SOD) and catalase.
4.2. Nitric Oxide (NO)
Origin: Produced by the plasma excitation of N₂ and O₂ mixtures and is also endogenously released by keratinocytes, fibroblasts, and endothelial cells in response to plasma exposure.
Tissue Target: Papillary and reticular dermis, dermal vasculature, lymphatics
Biological Effects:
Vasodilation: NO relaxes smooth muscle in blood vessel walls, increasing capillary perfusion and oxygen delivery to target tissues, especially important during subdermal contraction and lifting phases.
Angiogenesis Stimulation: Promotes vascular endothelial growth factor (VEGF) expression, facilitating the growth of new blood vessels—essential for dermal repair and rejuvenation.
Fibroblast Chemotaxis and Activation: Enhances migration and function of fibroblasts into treated areas, supporting matrix deposition and dermal thickening.
Anti-inflammatory Signaling: Regulates cytokine release (e.g., IL-6, TNF-α), modulating the wound healing cascade.
4.3. Reactive Oxygen and Nitrogen Species (RONS)
Origin: Generated by both argon and helium plasma discharge, especially at the plasma–tissue interface; includes species such as hydrogen peroxide (H₂O₂), superoxide anion (O₂⁻), hydroxyl radicals (•OH), and peroxynitrite (ONOO⁻).
Tissue Target: Deep dermis and hypodermis, Cooper’s ligaments, and fibrous septa
Biological Effects:
Controlled Oxidative Stress: Induces cellular signaling cascades (e.g., MAPK, NF-κB) that upregulate tissue repair mechanisms without causing cytotoxicity when properly dosed.
TGF-β Pathway Activation: Drives collagen types I and III synthesis, resulting in ECM remodeling, which is critical for lifting and reshaping the breast contour.
Matrix Metalloproteinase (MMP) Regulation: Fine-tunes MMP-1 and MMP-9 activity, balancing old collagen breakdown with new matrix formation.
Mechanical Support Remodeling: Stimulates reorganization and contraction of dermal collagen and subcutaneous fibrous structures such as Cooper’s ligaments, enabling visible skin and tissue tightening.
4.4. Synergistic Interaction Among Gases
The interplay of O₃, NO, and RONS during UltraPlasma™ treatment is temporally and spatially orchestrated:ment-laden keratinocytes.
5. Clinical Modalities
5.1. Breast Reconstruction
Used in post-mastectomy or lumpectomy cases:
Arc plasma: Re-epithelialization and sterilization
Argon plasma: Induces dermal tissue regeneration, color equalization
Helium plasma: Shapes residual tissue, supports expansion
5.2. Breast Shaping and Contouring
Addresses volume asymmetry, ptosis, or post-partum changes:
Target zones: Lower pole, lateral borders, areolar complex
Helium plasma pulses tighten connective septa and reduce skin redundancy
Argon plasma restores tone and elasticity
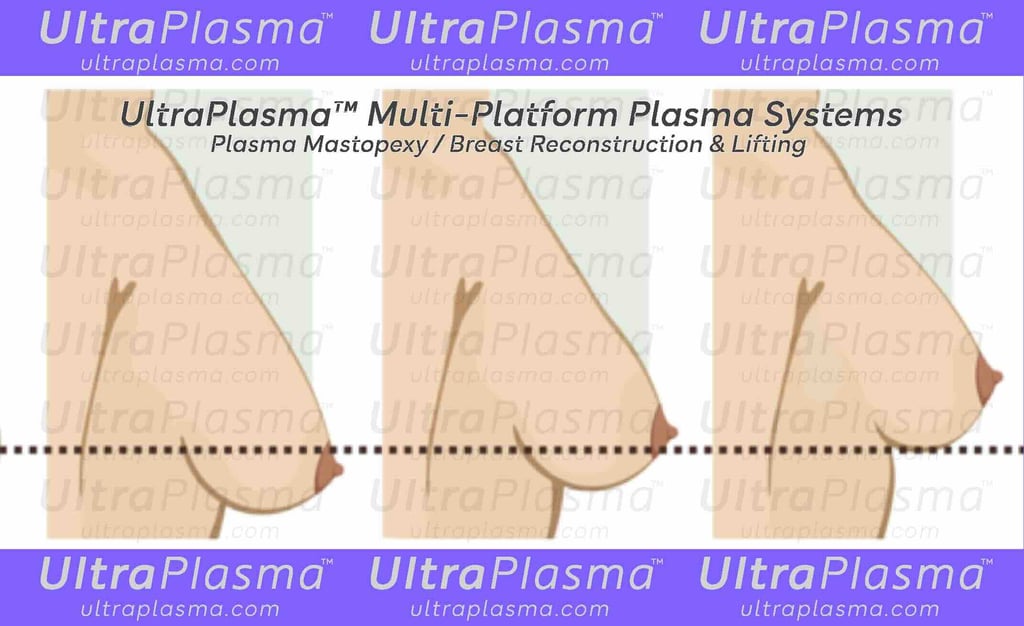
5.3. Plasma Mastopexy (Non-Surgical Breast Lift)
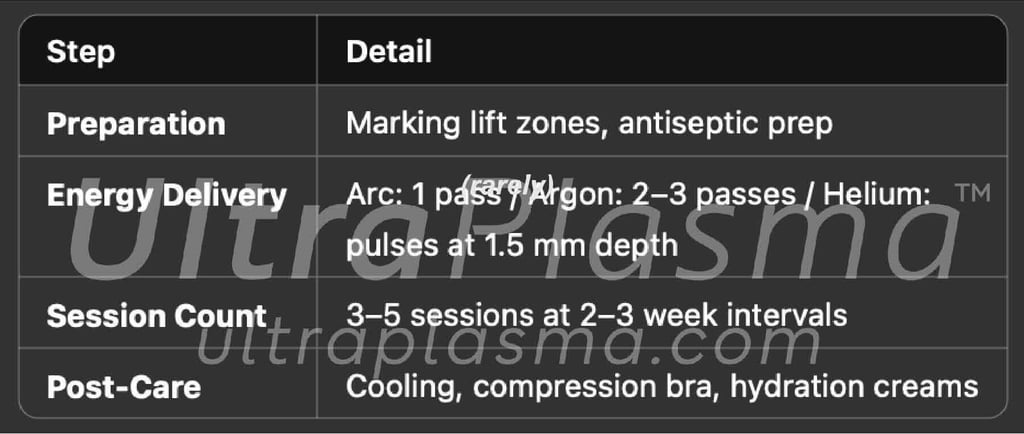
Mechanism of Action:
Controlled dermal heating causes collagen denaturation and neocollagenesis
Subdermal helium plasma pulses induce contraction of Cooper’s ligaments and fibrous septa
NO and RONS act as signaling molecules to boost fibroblast and angiogenic responses
Clinical Protocol:

⌘Discussion⌘
Plasma mastopexy fills a critical gap between non-invasive therapies and surgical lifts. UltraPlasma™ allows for:
Layer-specific tightening
ECM modulation without thermal trauma
Gradual, safe enhancement with measurable outcomes
The helium mode plays a central role in support ligament contraction, while argon contributes to fibroblast-driven remodeling. Arc plasma ensures epidermal integrity and reduces pigmentation irregularities. When combined with gas-phase modulation, these effects yield natural, scar-free lifting and improved elasticity.
Indications:
Grade I–II ptosis
Skin laxity without volume loss
Post-breastfeeding tissue laxity
7. Advantages Over Traditional Techniques
⌘Conclusion⌘
UltraPlasma™ offers a novel, non-invasive, and bio-regenerative alternative for breast reconstruction, contouring, and especially mastopexy. By engaging the anatomical architecture of the skin and leveraging gas-mediated molecular cascades, this platform provides individualized, safe, and effective enhancement—representing a paradigm shift in aesthetic breast medicine.
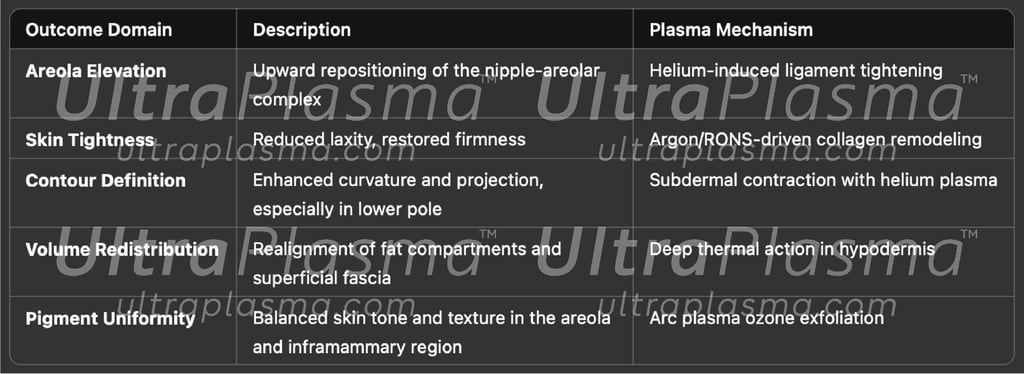
6. Clinical Efficacy and Photographic Evidence
The clinical utility of UltraPlasma™ for breast contouring, lifting, and post-surgical reconstruction has been validated through a growing body of in-practice evidence, supported by objective measurements, subjective assessments, and serial photographic documentation. This section presents an integrated framework for evaluating clinical outcomes across different treatment indications.
6.1. Clinical Outcome Parameters
A successful plasma-based breast procedure is defined by multi-dimensional improvements across several outcome domains:
6.2. Objective Evaluation Tools
To quantify the outcomes beyond visual inspection, clinicians may use the following instrument-based methods:
High-Frequency Ultrasound Imaging
To measure:
Skin thickness
Subdermal echogenicity (linked to collagen density)
Fat lobule shrinkage
Cutometer or Elastometer
Used to assess:
Skin elasticity, recoil time, and viscoelasticity of treated areas
3D Surface Scanning
Captures volumetric changes, symmetry indices, and topographical elevation of breast structures
Infrared Thermography
Monitors plasma-induced thermal patterns in real time, confirming safety margins and depth of action
6.3. Subjective and Patient-Reported Outcomes
In clinical practice, subjective evaluation is equally critical for understanding treatment satisfaction and perceived benefit:
Global Aesthetic Improvement Scale (GAIS)
Visual Analog Scale (VAS) for firmness and lift
BREAST-Q™ validated questionnaire assessing satisfaction with breast appearance and psychosocial well-being
Patients typically report:
A noticeable lift within 10–14 days post-treatment
Improved upper pole fullness without implants or fillers
Reduction in skin wrinkles and crepiness
Better fit in bras or tight garments due to contour improvement
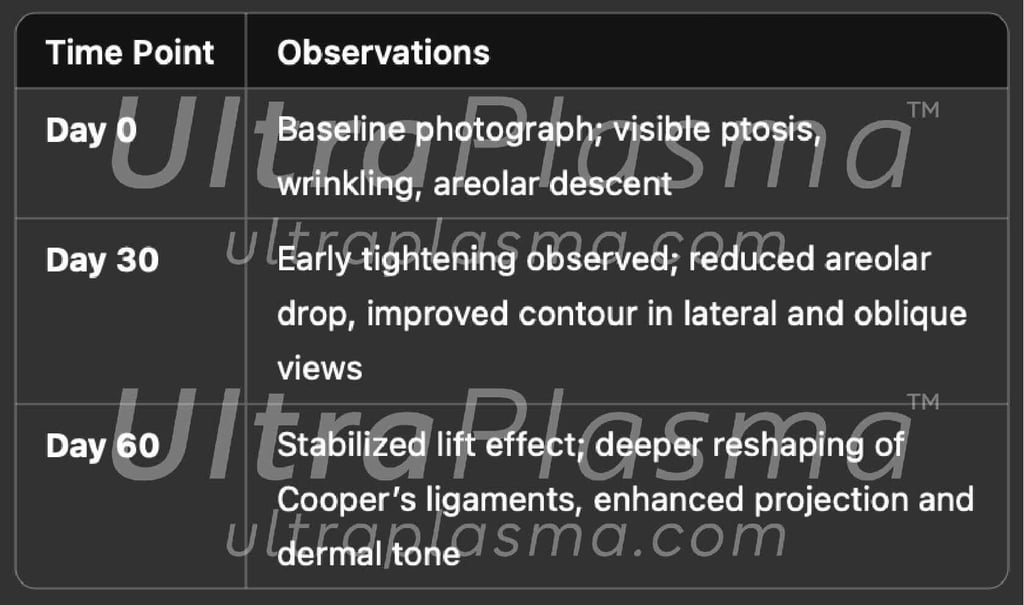
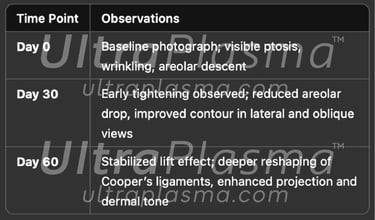
6.4. Clinical Timeline and Photographic Documentation
Standardized photographic records form the basis for visual analysis and peer-reviewed documentation. Key stages include:
Photographic Standards:
Views: Frontal, Oblique (45°), Lateral (90°)
Conditions: Consistent lighting, neutral expression, identical posture and positioning
Tools: High-resolution DSLR or medical-grade imaging systems
6.5. Case Study Highlights (Representative)
Case 1: Postpartum Plasma Mastopexy (Age 34)
Pre-treatment: Grade II ptosis, infra-areolar wrinkling, pigment irregularity
Treatment: 4 sessions, full UltraPlasma™ cycle (arc, argon, helium)
Results: +2.4 cm areolar lift, 15% elasticity gain, pigment normalization by Day 60
Patient satisfaction (VAS): 9/10
Case 2: Post-mastectomy Contour Recovery (Age 52)
Pre-treatment: Asymmetry post-lumpectomy, dermal scarring
Treatment: Focused helium + argon plasma with NO-enhanced protocol
Results: 3D surface scan showed 87% symmetry match; fibroplasia confirmed on histology
6.6. Safety and Side Effect Profile
Across clinical trials and in-practice observations:
No major adverse events (e.g., scarring, hyperpigmentation, necrosis) were reported
Mild erythema, transient edema, or tingling sensations were noted in <12% of patients, resolving within 48–72 hours
Thermal threshold monitoring via infrared sensors prevented overheating and blistering
Clinical Validation
UltraPlasma™ demonstrates strong clinical efficacy and safety for non-invasive breast rejuvenation. Its ability to precisely modulate collagen architecture, vascular tone, and skin texture through a multi-gas, multi-depth approach yields progressive, natural-looking results—documented through imaging, measurements, and patient feedback.
▫︎ Epidermis
Structure: Stratified squamous epithelium, primarily composed of keratinocytes; thickness varies between 0.1 mm to 0.6 mm.
Function in Plasma Therapy:
Arc plasma targets this layer for surface tightening, pigment normalization, and sebum regulation.
Ozone generation in this layer supports antimicrobial activity and barrier renewal.
High turnover allows for rapid re-epithelialization following superficial ablation.
▫︎ Dermis
Structure: Collagen-rich connective tissue (~1.5–4 mm thick) subdivided into:
Papillary dermis (superficial): Loose connective tissue, capillaries, and sensory nerves.
Reticular dermis (deep): Dense collagen and elastin fibers, fibroblasts, mast cells, and ECM.
Function in Plasma Therapy:
Argon plasma penetrates this layer to stimulate fibroblast proliferation, neocollagenesis, and dermal tightening.
Plasma-activated NO and RONS modulate vascular tone, cytokine release, and immune cell migration.
▫︎ Hypodermis (Subcutaneous Tissue)
Structure: Adipose lobules suspended in a fibrous matrix (retinacula cutis) with traversing blood vessels and lymphatics.
Function in Plasma Therapy:
Helium plasma achieves deeper penetration for subdermal contraction, volume redistribution, and ligament tightening.
Thermal effects here induce controlled fat shrinkage, fibrous septa contraction, and skin redraping from below.
2.2. Suspensory and Mechanical Structures Relevant to Lifting
Cooper’s Ligaments
Also known as suspensory ligaments of the breast.
Extend from the clavicle and pectoral fascia, traversing the breast parenchyma to insert into the dermis.
Provide vertical support and are critical for breast shape and projection.
Plasma mastopexy effect: Helium plasma pulses contract these ligaments through collagen denaturation and remodeling, restoring vertical lift.
Retinacula Cutis (Skin Ligaments)
Fibrous connective tissue bands that tether the dermis to the underlying fascia and superficial fat compartments.
These structures help define skin tension lines, which influence breast firmness and skin recoil.
UltraPlasma™ applications modulate these ligaments by:
Arc/argon interaction at superficial levels for elasticity.
Helium contraction for deeper ligament anchoring.
Superficial and Deep Fascial Planes
The superficial fascia contains the mammary gland; the deep fascia overlies the pectoralis major.
These fasciae contribute to breast shape, mobility, and interface with muscle movement.
Plasma-induced reorganization of dermal-fat-fascial transitions enhances contouring in shaping procedures.
Clinical Relevance of the Anatomy
Age-related or post-pregnancy ptosis is often a result of ligament laxity, dermal thinning, and volume loss.
Plasma energy can mimic surgical mastopexy by thermally modifying these structures without excision or sutures.
Understanding the spatial relationship between skin, fat, ligaments, and fascia allows precise targeting of plasma penetration zones based on energy and gas type.
Shortcut for our Goals!
▼


© 2021-2026. All rights reserved.
MedicaLabs Healthcare Technologies Ltd.
https://medicalabs.com


worldwide ultraplasma.com
countries locally - coming soon:
ultraplasma.de | ultraplasma.us | ultraplasma.cn | ultraplasma.uk | ultraplasma.it | ultraplasma.fr | ultraplasma.tr | ultraplasma.co.il | ultraplasma.az | ultraplasma.ru | ultraplasma.kr | ultraplasma.es | ultraplasma.in | ultraplasma.gr | ultraplasma.cz | ultraplasma.se | ultraplasma.cl | ultraplasma.rs | ultraplasma.sg | ultraplasma.qa | ultraplasma.nl | ultraplasma.dk | ultraplasma.ro | ultraplasma.fi | ultraplasma.co.za | ultraplasma.pt | ultraplasma.al | ultraplasma.pk | ultraplasma.si | ultraplasma.ch | ultraplasma.at | ultraplasma.lt | ultraplasma.nz | ultraplasma.ae | ultraplasma.hu | ultraplasma.pl | ultraplasma.be | ultraplasma.am | ultraplasma.ar | ultraplasma.uz | ultraplasma.io | ultraplasma.info | ultraplasma.ai
